
Many parents are concerned that their baby may be tongue-tied. Many breastfeeding problems are blamed on tongue-tie. Almost everyone has a lingual frenulum, or bit of tissue under the tongue that helps connect the tongue to the floor of the mouth. The most important thing is that the tongue can move properly.
Most breastfeeding problems are caused by misunderstanding what babies need. Help with positioning and latch is the first step to improving breastfeeding. LLL meetings, LC consultations, breastfeeding or baby cafes are all good resources for getting individualized help.
Some tongue-tied babies can make breastfeeding work. Even if your baby has an obvious tongue-tie, first get help from a lactation professional.
Most professionals agree that a tight frenulum that attaches to the tip of the tongue can make it more difficult for babies to feed. These tongue-ties can be easy to treat in a doctor or dentist's office. Figure 3 shows a very tight frenulum that experts agree needs treatment.
There is more controversy about babies who do not have good tongue mobility but do not have a tight frenulum at the front of the tongue. New anatomy research suggests that tight fascia (the soft tissue that joins body structures) may be responsible. Depending on the cause of the tightness, therapy may be the best option. Physical therapy is best studied for neck muscle imbalances caused by the baby’s position during pregnancy, other body work may be helpful as well.
Here's how you can look at your own baby's tongue movements:
The first thing to assess is whether your baby can stick out his or her tongue. If you touch your baby's lips, he will probably open his mouth. You can then touch the front of his lower gum with your fingertip. This makes him stick the tongue out. We want to see the tongue come out flat over the lip without denting or dimpling.

Next, we want to see if your baby can lift her tongue way up to the roof of the mouth. All the way up is perfect, half way is enough for most babies to be able to breastfeed. Again, her mouth should be open when you check if the tongue can lift up.

Tongue-ties:
This baby (figure 3) has an obvious tongue-tie. You can see the membrane right at the front of the tongue, and you can see how it makes it hard for him to lift his tongue up.

Babies with a tight frenulum may have a notch in the tip of the tongue when they try to move the tongue (figure 4). This is also called a "heart-shaped" tongue. Some babies have a notch but can still lift the tongue normally. Remember we want to look at the whole baby and not just one feature.

Babies with a tongue-tie will often raise the sides of the tongue while the front of the tongue pulls downward toward the floor of the mouth. Professionals call this a "low tongue posture". See (figure 5)

Babies with restricted or weak tongue movements will have a high, narrow roof of the mouth (figure 6). This is an important "double check" or confirmation that the tongue is not moving well. There are other reasons to have a high or narrow palate too, such as being in a position during development that prevented the baby's head from expanding side to side.

Having a shorter lower jaw than average can affect tongue strength. This baby (figure 7) does NOT have a tongue-tie. Dividing the frenulum when the real reason for sucking problems is a short jaw or muscle tightness in the face or neck will not help and can often make the problem worse.

Again, if your baby does seem to be tongue-tied, please get lactation help first. Some tongue-tied babies are able to breastfeed without treatment with some special help latching on. An IBCLC should also be able to help determine whether a breastfeeding problem is from a tongue tie or is from poor latch or positioning, a short jaw or tight muscles and communicate these findings with your baby's primary health care provider.
Snuggle your baby against your body so he is tummy to tummy (front to front) and lean back comfortably. Most mothers like to hold the baby with the same side arm as they are nursing from, or with both hands. The more you lean back, the more gravity helps hold baby, and the less strain on your arms.

Babies find the breast by feel and smell. Cuddle your baby in a comfortable position so your nipple touches that cute notch right above her upper lip, and her chin snuggles against your breast.

She will then open her mouth wide.

It will look like she won't be able to get her upper lip past the nipple.
She'll tilt her head back a little bit and lunge in for a good mouthful. If her nose is blocked, snuggle her bottom close to your body and slide her a little toward your other breast.

If this doesn't work for you, try leaning even farther back, so your nipple points up in the air. Then turn your baby so he is laying on your chest, with his face aligned to the breast the same way as in the latch photos above.

If you need to shape your breast a little to define a better mouthful, you can do this with one finger above or below the nipple, or a finger above and a finger below.

If these things don't work, express milk very frequently (at least 8 times a day) to feed your baby, and get in-person help!
Parents worry their baby isn't get enough milk when they seem to breastfeed constantly. Answering some simple questions can help reassure you or let you know to get breastfeeding help.
1. Is the baby having wet and dirty diapers?
New babies should have at least one wet and one poopy diaper for each day of life. One each on day 1, two each on day 2, 3 each on day 3. Poops start out thick and dark (see figure 1), and gradually become yellow, soft and more liquid with little curds by day 4-5.
By 5 days old, breastfed babies should have 5-6 wet diapers and 5 or more poops at least the size of a US quarter coin (or a euro or Canadian "loonie", or an Australian 2 dollar coin). Some babies have fewer but bigger stools.
2. Is baby relaxed after feeding?
On the second day of life, most babies breastfeed constantly to help increase the milk production. Babies bring their hands to their mouth when they are hungry (see figure 2).

Other than a single day of "feeding frenzy" on the second or third day of life, babies should relax and fall asleep after nursing. As they get a little bigger, they let go of the breast and either look for the other breast or put their head down to rest on you (see figure 3). So cute!

3. Does baby wake up to nurse?
Some newborns need a little help to wake up to feed. Holding them skin to skin (baby in a diaper, you topless, a blanket over baby's back if it's chilly) helps them wake up and smell the coffee, er, milk. It's actually a good sign if your baby wakes up every couple of hours, with one longer stretch of about 4 hours a day.
If the answer to all three questions was yes, all is probably fine. See this cool youtube video for what's normal: https://www.youtube.com/watch?v=Brhq-Z11zos.
If your baby is very sleepy and doesn't wake up to nurse, is having few poopy diapers (or only little skidmarks of stool or orange urine after day 3 - see figure 4), or cries every time he or she comes off the breast, get help!

Many International Board Certified Lactation Consultants (IBCLCs) are doing virtual consultations for new families during social isolation. You can visit http://www.nylca.org for help in NYC.
La Leche League Leaders are available on the telephone and some are having virtual meetings. More information can be found at LLLofqueens.com.
While you work to get help, try expressing extra milk and feeding with a spoon (see figure 5) or cup (see figure 6).See the links for parents for ways to get milk out with your own hand.

So far, small studies have not found the coronavirus (SARS CoV-2) that causes COVID-19 in the milk of mothers with the disease. Only one baby seems to have been born with the virus.
Human babies have very immature immune systems. Breast milk contains antibodies and other things that kill germs and strengthen baby's immune system. It is best to breastfeed with most illnesses.
During any emergency, supplies of infant formula can be disrupted. Many stores I've been to in the past few weeks have been completely sold out of formula. Formula does not provide support for the baby's immune system like human milk does.
Holding your baby skin to skin immediately after birth and breastfeeding in the first hour or two helps you make more milk than waiting to breastfeed until later.

If you are healthy when you give birth, get as much breastfeeding practice and help as you can while you are in the hospital. NYC hospitals have IBCLCs (International Board Certified Lactation Consultants) or CLCs (Certified Breastfeeding Counselors) to help you get off to a good start. Keep your baby with you in your room, and feed as often as baby asks. Early hunger signs include wiggling, moving the tongue, and bringing the hands to the mouth. Babies are more patient with learning to breastfeed when they are just a little hungry. If you need more help when you get home, many IBCLCs are doing virtual consults.
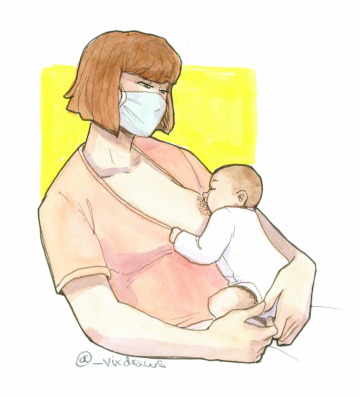
If you have symptoms that MIGHT be COVID-19 when you give birth, you should wash your hands very carefully before handling your baby or your breasts (figure 3), wear a mask while handling your baby, and while breastfeeding (figure 2) or skin to skin (figure 1).

If you DO have COVID-19 when you give birth, you might be separated from your baby in the hospital. You can still express your milk for someone healthy to give the baby until you recover. Practice the same handwashing, and wash your pump parts and other things you touch very carefully. If you are home, you can consider breastfeeding while wearing a mask and practicing careful handwashing before touching your baby. If you have been separated in the hospital, you will likely need help to transition to breastfeeding and increase your milk supply. Pumps are not as good as babies, especially in the first week! Many IBCLCs are offering virtual consultations to help you.
If you are already breastfeeding and get ill, your baby has already been exposed and you already have antibodies in your milk. It's wise to continue breastfeeding and to practice careful handwashing and wear a mask while handling your baby. Someone who is not ill can change diapers and cuddle baby so you can get some extra rest.
If you are still pregnant, learn how to express milk with your own hand. See links in Links for Parents. This works better in the first few days if your baby is separated from you. Keep any drops you get (ask your nurse for a sterile container) to spoon or syringe feed your baby. The more often you express in the first 3 days, the more milk you will make.
If you want to read the official statements of various professional organizations, here they are:
Academy of Breastfeeding Medicine
La Leche League
United States Breastfeeding Committee
US Centers for Disease Control and Prevention
World Health Organization
Thanks to Laura @_vixdraws for the beautiful drawings.
Home